Neuro-Optometry is a specialty field of vision care that combines neurology and optometry to assess how the brain processes information sent from the eyes. When communication between your brain and eyes are disrupted due to injury or disease vision problems usually occur.
Each year, more than 1 million people sustain traumatic brain injuries. 90% of head trauma survivors need visual care. There are many illnesses and injuries that can have dramatic effects on the visual system. Traumatic head injuries, stroke, prolonged illness and diseases can cause problems in the visual system. The results can be problems with eye teaming, tracking, diplopia (double vision), perceptual and/or focusing problems.
When should assessment occur?
Due to the impact of the visual system on cognitive and motor function, the visual rehabilitative needs of the brain injured, stroke or neurologically impaired patient must be addresses as early as possible and should be referred to a Neuro-optometrist for further evaluation.
Post Concussion / Traumatic Vision Syndrome or Visual Midline Shift Syndrome and patients with their associated symptoms are indications for possible Neuro-optometric rehabilitation. Please take our Post Concussion / Brain Injury Symptom Checklist or contact us for more information or to set up a Neuro-Visual processing evaulation.
Post Concussion / Traumatic Vision Syndrome
The visual process is part of a sensorimotor feedback loop, which includes kinesthetic, proprioceptive and vestibular processes. Insults to the cortex produced by an acquired brain injury or stroke cause stress or interference in the central and autonomic nervous systems. As a result, a brain-injured person may experience diplopia, binocular dysfunction, or concentration 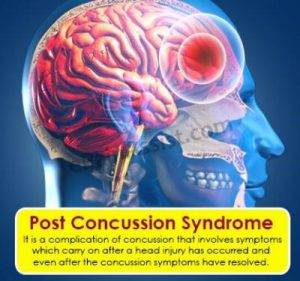 difficulties. In the past, these symptoms were diagnosed as individual eye problems or muscle imbalances. We now know that these eye problems and other reported difficulties that result from a brain injury often occur because of the interference in the visual process. This, in turn, will cause sensorimotor spatial disorganization. This may also cause an eye to turn out or a strong tendency for both eyes to diverge. The resulting binocular problems are characteristic of Post Concussion / Traumatic Vision Syndrome.
difficulties. In the past, these symptoms were diagnosed as individual eye problems or muscle imbalances. We now know that these eye problems and other reported difficulties that result from a brain injury often occur because of the interference in the visual process. This, in turn, will cause sensorimotor spatial disorganization. This may also cause an eye to turn out or a strong tendency for both eyes to diverge. The resulting binocular problems are characteristic of Post Concussion / Traumatic Vision Syndrome.
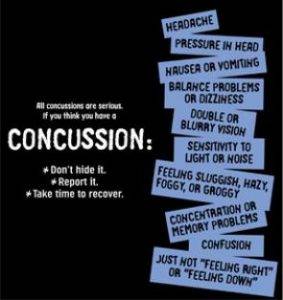
Symptoms of Post Concussion / Traumatic Vision Syndrome:
• Double vision
• Headaches
• Blurred vision
• Dizziness or nausea
• Light sensitivity
• Attention or concentration difficulties
• Staring behavior (low blink rate)
• Spatial disorientation
• Losing place when reading
• Can't find beginning of next line when reading
• Comprehension problems when reading
• Visual memory problems
• Pulls away from objects when they are brought close to them
• Exotropia or high exophoria
• Accommodative insufficiency
• Convergence insufficiency
• Poor fixations and pursuits
• Unstable peripheral vision
• Associated neuromotor difficulties with balance, coordination and posture
• Perceived movement of stationary objects
Visual Midline Shift Syndrome
Visual Midline Shift Syndrome is an unusual phenomenon that often occurs following a neurological event such as a TBI or CVA. The ambient visual process
changes its orientation with regard to the midline of vision. Both lateral and
transverse midlines can be affected. We use the parietal lobe to integrate all
sensory input, including vision, and to be able to interpret information for
functional use. Visual input from the left eye is processed in the right side of the
brain, and input from the right eye is processed in the left side of the brain. When
this process is altered after a neurological event or injury, it can create a
perceived amplification of space internally on one side and a compressed
amplification of space on the other.
Symptoms of Visual Midline Shift Syndrome:
• Dizziness or nausea
• Spatial disorientation
• Consistently stays to one side of hallway or room
• Bumps into objects when walking
• Poor walking or posture: leans back on heels, forward, or to one side when
walking, standing or seated in a chair
• Perception of the floor being tilted
• Associated neuromotor difficulties with balance, coordination and posture
When should assessment occur?
Due to the major impact of the visual system on cognitive and motor function , the
visual rehabilitative needs of the brain injured, stroke, or neurologically impaired
patient must be addressed as early as possible.
Help with Assessment
These guides and checklists have been prepared to assist patients and
rehabilitation professionals in determining the appropriateness of referring
persons who have sustained a traumatic brain injury, CVA or other neurological
impairment. This information should be used as a first step in determining if visual difficulties are interfering with the rehabilitation progress of the individual. Please take our Post Concussion / Brain Injury Checklist or contact us for more information or to set up a Neuro-Visual processing evaluation.